Notification
Please fill in the information below
Urgent
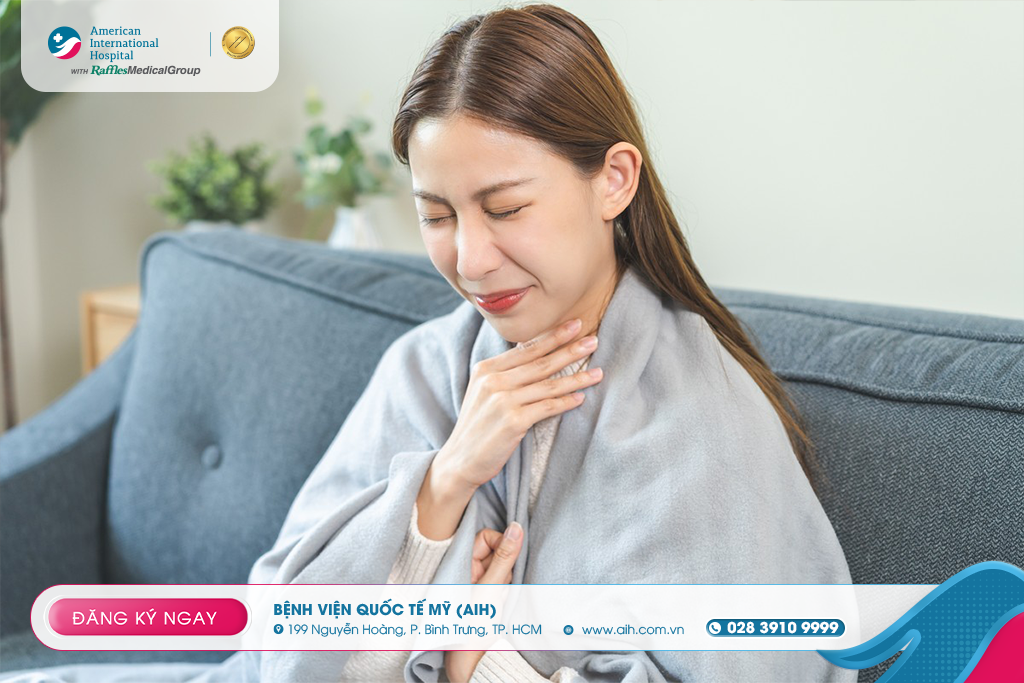
IS IT MANDATORY TO TREAT PHARYNGITIS WITH ANTIBIOTICS?
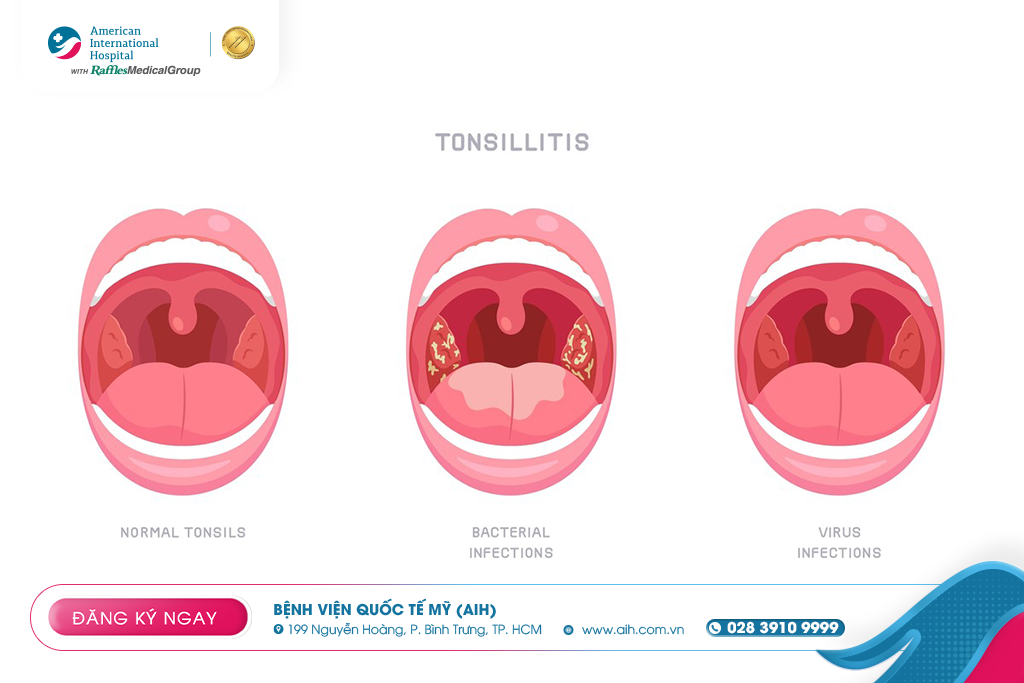
Pharyngitis is an inflammation of the back of the throat, often causing pain, a feeling of obstruction, or a burning sensation when swallowing. In many cases, pharyngitis occurs concurrently with tonsillitis when the tonsillar tissue is primarily inflamed or the inflammation spreads to the pharyngeal area.
Although most cases of pharyngitis are benign, pathogenesis, management, and prognosis depend on the cause, it is one of the most common reasons why patients, including both adults and children, seek consultation with an ear-nose-throat specialist.
Classification
Pharyngitis can be classified in several ways, depending on its duration, cause, and clinical severity:
1. By duration
Acute pharyngitis: rapid onset, progressing over several days to a week.
Chronic / recurrent pharyngitis: symptoms persist or recur multiple times a year, often associated with chronic irritants such as rhinosinusitis, gastroesophageal reflux, smoking, or repeated infections.
2. By cause
Viral pharyngitis (most common).
Bacterial pharyngitis (most commonly Group A Streptococcus).
Fungal / candidal pharyngitis — rarer, often seen in immunocompromised individuals or those on prolonged antibiotic therapy.
Pharyngitis due to other causes such as chemical irritation (smoke, toxic gases), allergies, acid reflux, or underlying medical conditions.
3. According to the nature of the physical lesion
Erythematous pharyngitis: the pharyngeal mucosa is red and edematous.
Membranous pharyngitis: The presence of purulent membranes or pseudomembranes on the pharyngeal mucosa, often due to bacterial infection or superinfection.
Ulcerative pharyngitis: Characterized by ulcers or lesions in the throat area, sometimes accompanied by hemorrhage. Possible causes include virus, herpes simplex virus, or specific causes.
Pharyngotonsillitis
When both the pharynx and tonsils are inflamed simultaneously, the manifestations may lean towards the tonsils (e.g., pus, swollen tonsils), but the essence is still a combined inflammatory lesion.
Causes
Virus
Viruses are the primary cause of pharyngitis. Viruses often lead to widespread inflammation, accompanied by other upper respiratory tract inflammation symptoms such as runny nose, sneezing, coughing, and fatigue.
Bacteria
The main bacterium causing pharyngitis is Streptococcus pyogenes (Group A Streptococcus, GAS), a condition known as streptococcal pharyngitis. Other less common bacteria include Neisseria gonorrhoeae, Chlamydia pneumoniae, and Mycoplasma spp.
Fungi (Candida spp.)
Rare and typically occur in individuals with compromised immune systems, chronic respiratory diseases, or those undergoing prolonged antibiotic or corticosteroid treatment.
Mechanical / Chemical / Allergic / Reflux Causes
Tobacco smoke, chemical fumes, dry air, and gastroesophageal reflux disease (GERD) can irritate and cause chronic inflammation of the pharyngeal mucosa. In some cases, pharyngitis can be a symptom of newly acquired HIV infection.
Predisposing factors and transmission
Viral and bacterial pharyngitis are transmitted through droplets or close contact (talking, coughing, sneezing).

Symptoms
The symptoms of pharyngitis largely depend on the causative agent and the degree of inflammation. Below are common symptoms and signs suggestive of bacterial infection.
Main symptoms
Sore throat, burning throat, a feeling of obstruction when swallowing (odynophagia).
Dry throat, itchy, dry, gritty sensation.
Fever (can be mild or high depending on the cause).
Headache, fatigue, muscle aches, poor appetite, sometimes nausea or abdominal pain (especially in children).
Pharyngitis may be accompanied by rhinosinusitis, cough, runny nose if it is a viral infection.
Upon examination, the pharyngeal mucosa appears red, edematous, possibly with pseudomembranes or pus on the tonsils, anterior cervical lymphadenopathy, red membrane, or petechiae on the palate.
Warning symptoms requiring urgent medical attention
Increasing difficulty swallowing
Significant neck swelling, throat swelling causing difficulty breathing
Drooling, inability to chew or swallow
Blood in sputum or throat secretions
Symptoms lasting > 7 days without improvement

Diagnosis
The diagnosis of pharyngitis is not solely based on clinical findings but requires targeted tests to differentiate the cause and determine treatment:
1. Clinical examination and history
The doctor will observe the pharyngeal mucosa (degree of redness, swelling, pseudomembrane, pus), palpate cervical lymph nodes, assess accompanying respiratory tract inflammation signs (nose, sinuses, ears), inquire about onset, accompanying symptoms (cough, nasal congestion, runny nose), and risk factors (contact with other patients, history of recurrent pharyngitis, use of immunosuppressants).
2. Rapid antigen detection test (RADT)
Specifically for detecting Group A Streptococcus. If positive, the doctor may initiate antibiotic treatment. If negative, in many cases, a culture is still necessary to avoid missing bacterial infections.
3. Throat culture
If the RADT is negative or other bacteria are suspected, a culture will help accurately identify the bacteria and assess antibiotic susceptibility (for severe or recurrent cases).
4. Ancillary tests based on specific suspicions
If mono (EBV) is suspected: serological tests (e.g., Monospot).
If there are systemic symptoms or newly acquired HIV is suspected, an HIV test should be performed.
In cases of suspected fungal infection: fungal culture or direct microscopy.
If complications are present (peritonsillar abscess, widespread pus), an otorhinolaryngoscopy or neck CT scan may be necessary.
5. Endoscopy / Laryngoscopy
In some difficult-to-diagnose cases (such as chronic pharyngitis, suspected physical lesions in the pharynx), an ENT doctor may use a flexible endoscope to observe the deep pharyngeal area and detect other lesions (tumors, polyps, chronic inflammation).
Selecting tests based on clinical probability (Centor criteria) and patient context (age, severity, risk) is important to avoid antibiotic overuse.

Treatment
The treatment strategy for pharyngitis comprises two main approaches: symptomatic treatment (in most viral cases) and specific treatment when a bacterial cause is identified.
1. Symptomatic/Supportive treatment
Rest, drink plenty of fluids to help rehydrate and reduce mucosal irritation.
Gargle with warm salt water to reduce inflammation and soothe the throat lining.
Pain relievers/fever reducers: acetaminophen (paracetamol), ibuprofen, or naproxen (if not contraindicated).
Throat lozenges, humidifiers, avoid irritants such as smoke and dust.
2. Antibiotics (if bacterial cause, especially Group A Streptococcus)
When tests confirm Group A Streptococcus or if there's a high risk (based on clinical criteria + tests), antibiotics are indicated to reduce symptom duration, limit spread, and prevent complications (glomerulonephritis, carditis, rheumatoid).
Standard therapy is typically penicillin or amoxicillin.
In patients allergic to penicillin, macrolides or cephalosporins may be used (depending on the situation, based on sensitivity).
Ensure correct dosage and duration to avoid treatment failure or recurrence.
3. Surgical / Interventional treatment
If tonsillitis/pharyngitis recurs frequently and medical treatment is ineffective, tonsillectomy may be considered.
The decision for surgery should be thoroughly evaluated by an ENT specialist, considering the benefits, risks, and impact on quality of life.
4. Monitoring and preventing recurrence
During treatment, if the patient’s condition does not improve after 48–72 hours or shows signs of worsening, a follow-up examination is necessary for reassessment, which may include repeat bacterial cultures or other tests.
For cases of chronic pharyngitis or frequent recurrence, it is essential to address predisposing factors such as rhinosinusitis, gastroesophageal reflux, dry environments, and to avoid smoking.
Maintaining respiratory hygiene: cover your mouth when coughing, wash hands frequently, and avoid close contact with sick individuals.
Reference:
--------------------




























































Leave a comment