Thông báo
Vui lòng điền vào thông tin bên dưới
Khẩn cấp
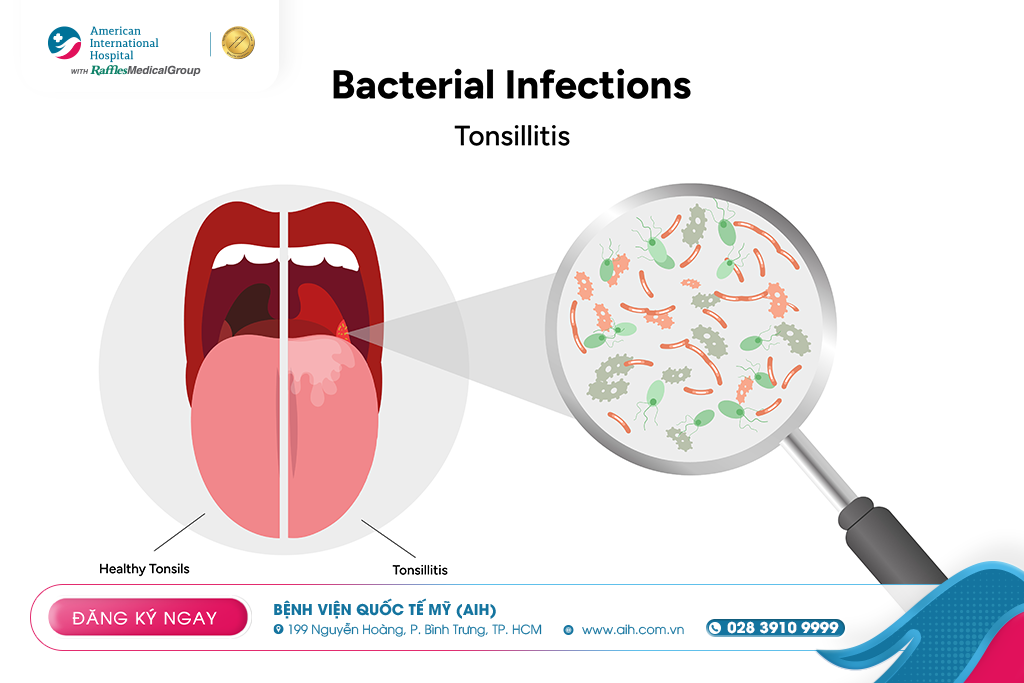
WHAT TO DO TO REDUCE PAIN EFFECTIVELY AND RECOVER QUICKLY FROM TONSILLITIS?
The tonsils are two lymphoid structures located bilaterally on the posterior pharyngeal wall, functioning as part of the lymphatic system of the oropharynx. This helps capture and mount immune responses against microorganisms that are inhaled or swallowed.
Tonsillitis is an acute or chronic inflammation of the tonsillar tissue, usually caused by infection, leading to swelling, redness, and sometimes purulent discharge or pseudomembrane formation.
Tonsillitis is a common condition, especially in children and adolescents, and can recur multiple times, affecting quality of life, nutrition, and occasionally leading to local or systemic complications.
Classification
Tonsillitis can be classified in several ways:
1. By duration of progression
Acute tonsillitis: rapid onset, lasting from a few days to less than 2 weeks.
Subacute/prolonged tonsillitis: lasting more than 2 weeks or not fully resolving.
Chronic/recurrent tonsillitis: occurring multiple times a year or persisting for many years.
2. By causative agent
Viral tonsillitis
Bacterial tonsillitis
Mixed tonsillitis (virus + bacteria)
3. By clinical presentation / complications
Uncomplicated tonsillitis
Tonsillitis with local complications (e.g., peritonsillar abscess)
Tonsillitis causing systemic / secondary complications (less common)
Causes
Microorganisms
Viruses: the most common cause of tonsillitis, including respiratory viruses such as adenovirus, rhinovirus, coronavirus, influenza virus, respiratory syncytial virus (RSV), etc. (similar to the pathogens seen in pharyngitis)
Bacteria: when bacteria invade and cause inflammation, the most common is Streptococcus pyogenes (Group A Streptococcus) (also commonly seen in acute pharyngitis).
Other bacteria: less common; mixed organisms or other bacteria may be involved depending on the clinical context.
Predisposing factors
Exposure to infectious sources (via droplets, oropharyngeal contact)
Reduced mucosal immunity in the throat
Concurrent upper respiratory tract infection
History of lymphadenitis in the oropharyngeal region
Poor respiratory hygiene conditions
Symptoms
The clinical symptoms of tonsillitis may vary depending on the severity of inflammation and the causative agent. Some common symptoms include:
Fever
Sore throat
Red, swollen tonsils
White or yellow purulent discharge on the surface of tonsils
Bad breath
Loss of appetite
Ear pain (may radiate to the ear)
Hoarse voice, throat itchiness, sensation of throat blockage
In young children: may present with vomiting, abdominal pain, and increased saliva secretion compared to usual

If the tonsillitis is recurrent or severe, there may be external signs such as swollen cervical lymph nodes, enlarged tonsils obstructing the airway, or complications like peritonsillar abscess causing nasopharyngeal deviation, difficulty opening the mouth, and severe pain.
Diagnosis
The diagnosis of tonsillitis is primarily clinical, with additional tests performed when necessary to identify the causative agent and rule out serious conditions.
Clinical examination
Inspect the tonsils: assess size, swelling, redness, presence of pseudomembrane or purulent discharge
Examine the nasopharynx, base of tongue, and cervical lymph nodes
Observe for difficulty swallowing, trismus, or nasopharyngeal deviation (if peritonsillar abscess is present)
Check temperature, pulse, and systemic signs
Supporting tests
Group A Streptococcus rapid antigen test (rapid strep test): if positive, streptococcal infection can be confirmed
Throat culture: performed when bacterial identification or antibiotic sensitivity testing is needed
Complete blood count, CRP / ESR: to assess the inflammatory response
Blood gas or blood oxygen: if there are signs of respiratory compromise
Nasopharyngoscopy: to evaluate deeper lesions, extension of inflammation, or suspected abnormalities in the throat

Differential diagnosis and considerations
Pharyngitis without tonsillar involvement
EBV infection / mono (mono can cause severe tonsillitis with pseudomembrane)
Tumors of the throat region; unilateral abnormal tonsillar enlargement (biopsy is recommended if one tonsil is abnormally large)
Peritonsillar abscess
Other causes of sore throat (e.g., antibiotic resistance, chemical/fungal-induced mucosal inflammation)
Treatment
Treatment of tonsillitis depends on the cause (viral or bacterial), the severity of symptoms, recurrence frequency, and the presence of complications.
Medical management
Supportive care:
Adequate rest
Hydration; soft, easy-to-swallow diet
Gargling with warm saline
Pain relievers and antipyretics (such as paracetamol, ibuprofen)
Antibiotics
For Group A Streptococcal tonsillitis, antibiotics should be used according to guidelines.
If bacterial infection is suspected and the rapid test is positive or the culture is positive, appropriate antibiotics should be given. If the cause is bacterial, the doctor will prescribe antibiotics; if it is caused by a virus, antibiotics are ineffective and the condition will resolve on its own.
Management of complications:
If a peritonsillar abscess develops, drainage is required and sometimes stronger antibiotics are needed.
If there is respiratory compromise / airway obstruction, emergency management is required.

Surgery (tonsillectomy)
Tonsillectomy is considered in the following situations:
Recurrent tonsillitis meeting criteria (≥ 5 episodes/year, or ≥ 3 episodes/year for 2 consecutive years, or ≥ 2 episodes/year for 3 consecutive years).
Chronic tonsillitis not responding to medical treatment.
Recurrent complications such as peritonsillar abscess or airway obstruction (e.g., markedly enlarged tonsils).
Unilateral tonsillar enlargement should be removed for biopsy to rule out malignancy.
Reference:
--------------------
Tìm kiếm
Tin tức
Bác sĩ





























































Để lại bình luận