Thông báo
Vui lòng điền vào thông tin bên dưới
Khẩn cấp
ESOPHAGEAL CANCER: EARLY IDENTIFICATION OF RISK FACTORS AND PREVENTIVE MEASURES
Esophageal cancer is one of the gastrointestinal cancers with a poor prognosis if detected late, with the sixth-highest mortality rate among cancers worldwide. Esophageal cancer tends to be more common in men, especially in countries with high rates of smoking and alcohol consumption.
Esophageal cancer not only severely affects the quality of life but also requires a multimodal treatment strategy to improve the prognosis.
► What is esophageal cancer?
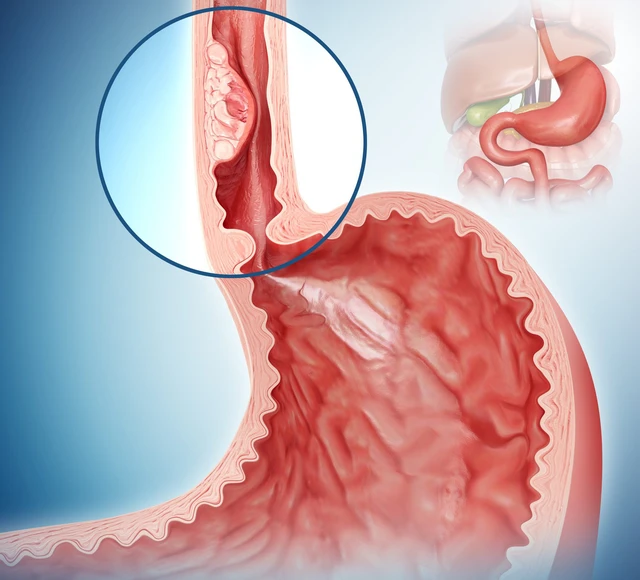
Esophageal cancer is a malignant tumor arising from the cells lining the lumen of the esophagus. There are two common types:
Squamous Cell Carcinoma (SCC): originates from squamous cells in the esophageal mucosa, commonly found in the middle and upper sections of the esophagus. This type is closely linked to smoking and alcohol consumption.
Adenocarcinoma (AC): originates from mucus-secreting glands, typically develops in the lower section of the esophagus and is associated with gastroesophageal reflux disease and Barrett's esophagus.
Besides the two main types, some rare forms such as small cell carcinoma, sarcoma (connective tissue cancer), lymphoma (lymphatic system cancer), and melanoma (melanocyte cancer) can also occur, but are very rare.
► Causes and high-risk factors
Age: Risk increases with age, especially after 50 or 60 years old.
Gender: Men have a higher risk of esophageal cancer than women.
Smoking: Is a leading risk factor for both main types of esophageal cancer (squamous cell carcinoma and adenocarcinoma).
Alcohol consumption: Drinking a lot of alcohol, especially when combined with smoking, significantly increases the risk, especially squamous cell carcinoma.
Chronic gastroesophageal reflux disease (GERD): Frequent reflux of stomach acid into the esophagus can damage the lining and lead to Barrett's esophagus, a significant risk factor for adenocarcinoma.
Barrett's esophagus: A condition in which the cells lining the lower esophagus are replaced by cells similar to those in the intestine. This is a complication of chronic GERD and is a strong precancerous lesion for adenocarcinoma.
Obesity: Increases the risk of esophageal adenocarcinoma, which may be related to an increased risk of GERD and other inflammatory changes.
Diet:
- Diet low in fruits and vegetables.
- High consumption of processed meats.
- Regularly drinking very hot beverages (which can cause thermal damage to the esophagus). (These aspects are often noted by both organizations)
Family history of esophageal cancer: Although not a major risk factor, it may play a small role

► Clinical symptoms
In the early stages, esophageal cancer is often silent and without obvious symptoms. As the tumor grows, typical symptoms include:
Progressive difficulty swallowing, initially with solid foods, then with liquids.
Unexplained weight loss.
Pain or burning sensation behind the sternum.
Prolonged heartburn, feeling of food getting stuck.
Persistent cough, hoarseness (if the tumor spreads to the vocal cords).
Vomiting blood or black stools if there is gastrointestinal bleeding.
These symptoms usually only appear when the disease has progressed, therefore early detection plays a key role.
► Diagnostic methods
The diagnosis of esophageal cancer usually begins with the doctor taking a medical history, family history, and performing a clinical examination. If there is suspicion, the diagnosis of esophageal cancer is based on a combination of clinical findings and modern paraclinical methods:
Esophagogastroduodenoscopy (EGD): is the fundamental method for direct observation of the mucosa and biopsy of suspected lesions.
Histological biopsy: confirms the diagnosis and determines the histological classification.
Endoscopic ultrasound (EUS): helps to assess the depth of invasion into the esophageal wall and the status of adjacent lymph nodes.
CT scan of the chest and abdomen: to assess lymph node or distant organ metastasis.
PET/CT: is valuable in assessing metastasis and treatment planning

► High-risk individuals
Some population groups need close monitoring because they are at high risk of developing esophageal cancer, including:
Men over 60 years old
People who smoke and/or drink alcohol for many years.
Patients with a history of long-term GERD (previously has or currently has gastroesophageal reflux disease), especially when there is Barrett's esophagus.
People with long-term obesity
Patients with achalasia (people with achalasia, a rare motility disorder of the esophagus) or a history of chest radiation therapy
Poor diet, low in fruits and vegetables.
Early identification of high-risk groups helps to enhance screening and detect cancer at an earlier stage.
► Treatment methods
Treatment for esophageal cancer depend on the stage of the disease, the location of the tumor, the histological type, and the overall condition of the patient. The main methods include:
Esophagectomy: This is the primary treatment for localized cancers and can be performed via open surgery, endoscopy, or robotic surgery.
Chemotherapy and radiotherapy: Applied alone or in combination, before or after surgery, especially in cases of advanced disease or when surgery is not possible.
Immunotherapy: This is a new advancement in the treatment of esophageal cancer, especially in the metastatic stage or when resistant to chemotherapy.
Targeted therapy: Directly targets abnormal molecules such as HER2 – a receptor often proliferated in adenocarcinoma, to inhibit the growth of cancer cells.
Supportive care: including nutrition, pain management, and psychological support, plays an important role in improving the quality of life for patients.
► New medical advancements
Some notable advancements in the diagnosis and treatment of esophageal cancer that are being researched and applied include:
Early detection using biotechnology: such as biomarker tests (biomarker tests) from esophageal mucosal samples to help detect cancer from the pre-clinical stage.
Minimally invasive surgery: application of endoscopic or robotic techniques to reduce post-operative pain and shorten recovery time.
Advanced immunotherapy: using monoclonal antibodies to enhance the activity of the immune system, improving treatment outcomes in patients with metastatic cancer.
► Esophageal cancer prevention
Esophageal cancer can be prevented through lifestyle changes and controlling risk factors:
Stop smoking and limit alcohol consumption.
Control body weight, avoid obesity.
Control gastroesophageal reflux disease (GERD) well and undergo regular endoscopy to detect early Barrett's esophagus lesions.
Increase a diet rich in green vegetables, fruits, and fiber.
Avoid consuming very hot food or drinks frequently.

► Esophageal cancer screening with advanced endoscopic techniques
Esophageal cancer is one of the dangerous malignant diseases, often detected late and has a poor prognosis if not diagnosed early and treated properly. However, thanks to the advancements of modern medicine, including early diagnostic endoscopy techniques, advanced imaging technology, and intensive treatment methods, thereby early detection and effective treatment, contributing significantly to improving the quality of life and prognosis for patients.
Esophagogastroduodenoscopy (EGD) is currently the optimal method for directly observing the esophageal lining, detecting early abnormalities such as inflammation, ulcers, pre-cancerous lesions, and early-stage cancer. Endoscopy also allows for the biopsy of damaged tissue to determine the cellular nature, thereby aiding in accurate diagnosis and appropriate treatment guidance.
Many studies show that if detected at an early stage, the 5-year survival rate of patients with esophageal cancer can reach 80-90%. Meanwhile, if detected at a late stage, this rate decreases to below 20%.
At the American International Hospital (AIH), with the Olympus endoscopy system featuring an automatic lesion staining mode using electronic optical mode, we implement a comprehensive strategy to prevent and detect early esophageal cancer. In this, endoscopy techniques play a key role, especially for high-risk individuals such as patients with chronic gastroesophageal reflux, people with Barrett's esophagus, or those with a history of smoking and long-term alcohol use.
If esophageal cancer is detected at an early stage, an endoscopist can remove the cancerous lesion via endoscopy without the need for surgery, helping to preserve esophageal function, and the patient will avoid a surgery, optimizing treatment outcome.
If you are in a high-risk group for esophageal cancer, such as having a history of chronic gastroesophageal reflux, Barrett's esophagus, or long-term smoking and alcohol consumption habits, proactive periodic screening is extremely necessary. Don't wait until symptoms appear to seek medical attention; protect your health today to detect the disease early and treat it promptly.
Register for esophageal cancer screening. Please contact Hotline (028) 3910 9999 or send message to https://m.me/aih.com.vn for detailed consultation.
--------------------
Tìm kiếm
Tin tức
Bác sĩ




























































Để lại bình luận