Thông báo
Vui lòng điền vào thông tin bên dưới
Khẩn cấp
DIABETES & THE ENDOCRINE SYSTEM: A CLOSE RELATIONSHIP
The endocrine system is a network of hormone-secreting glands, such as the pancreas, thyroid gland, adrenal glands, pituitary gland, etc., responsible for regulating metabolism, energy balance, glucose homeostasis, stress response, and many other physiological functions. When endocrine function becomes disrupted, glucose regulation may be impaired, leading to or worsening diabetes.
Type 2 diabetes mellitus (T2DM) is a metabolic disease characterized by insulin resistance and impaired pancreatic β-cell function. This demonstrates that endocrine factors play a central role in its pathogenesis. In addition, other hormones such as cortisol (from the adrenal glands), thyroid hormones, growth hormones (GH), and adipokines (substances secreted by adipose tissue) such as leptin and adiponectin also contribute to the regulation of glucose levels and metabolism.
The role of the endocrine system in the developmental mechanism and progression of diabetes mellitus
Type 2 diabetes mellitus is not simply a “blood sugar disorder,” but a disorder of the entire endocrine–metabolic system.
The pancreas, liver, adipose tissue, thyroid hormones, adrenal hormones, and even sex hormones all participate in regulating insulin and glucose.
Therefore, managing diabetes requires endocrine–metabolic expertise, aiming to achieve a comprehensive patient approach, rather than focusing only on blood sugar control.
The endocrinologist acts as a “conductor” in diabetes treatment:
Comprehensive endocrine-metabolic assessment: not only assesses blood sugar level, but also screens for thyroid disorder, Cushing syndrome, obesity, dyslipidemia, and renal diseases.
Personalised treatment: selecting hypoglycemia medication based on the endocrine-cardiovascular-renal profile of each patient. For example, prioritizing GLP-1 RA for overweight patients, and SGLT2i for those with heart/kidney failure.
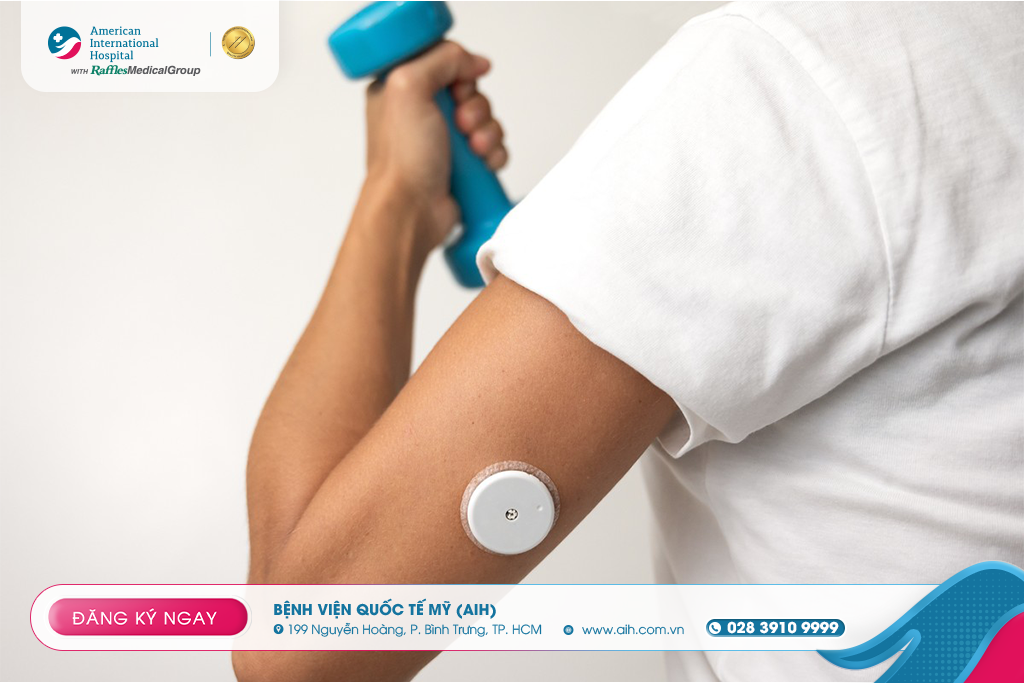
Technological application: Utilising the Continuous Glucose Monitoring (CGM) system and telemedicine for continuous patient care, reducing complications of hypo/hyperglycemia.
Multidisciplinary coordination: the endocrinologist acts as a bridge connecting cardiologist, nephrologist, ophthalmologist, nutritionist, and psychologist to monitor patients comprehensively.

The connection between diabetes mellitus and other endocrine disorders
Some common mechanisms that show the endocrine system has an impact on diabetes mellitus:
Thyroid hormones: Hyperthyroidism increases the rate of metabolism and glucose utilization, triggering glucose disorders; hypothyroidism could decrease metabolism and improve insulin resistance.
Adrenal hormones (cortisol, catecholamines): During chronic stress, elevated cortisol increases gluconeogenesis (glucose production) and insulin resistance.
Growth Hormones (GH) / IGF-1: influence glucose metabolism, might increase blood sugar level if homeostasis is not achieved.
Adipokine (leptin, adiponectin): from adipose tissue, regulating satiety/hunger and insulin sensitivity. “Inflamed” adipose tissue could release cytokines that cause insulin resistance.
Sex hormones (Testosterone, estrogen): in both men and women, the sex-hormone imbalance could be associated with insulin resistance and increased visceral fat.
Therefore, monitoring and managing hormones (thyroid, adrenal, sex, etc.) are inseparable parts in caring for patients with diabetes mellitus.

Prevention is key: high-risk patients (overweight, family history of diabetes, limited physical activities) could attend periodic endocrine follow-up to detect blood sugar disorders early.
Flexible blood sugar monitoring: Allows patients to monitor blood sugar easily, which could, in turn, help them adjust their daily diet and activities.
Comprehensive care: not only controlling blood sugar, but also monitoring blood pressure, blood lipid, renal function, eyes, and peripheral neurology. This is because they are significant endocrine-metabolic complications.
Personalized health education: every patient will receive consultations regarding diet, exercise, and stress management regimens tailored to their work, habits, and culture.
The endocrine system plays a vital role in preventing and managing diabetes mellitus.
How can we prevent and manage it effectively?
1. Early prevention
Maintaining healthy weight, especially waist circumference.
Having balanced diet: Limit refined sugar consumption; increase intake of green vegetables, whole grains, fish, and healthy fat.
Doing exercises: at least 150 minutes/week of fast jogging, swimming, cycling; combined with resistance training to increase muscle mass.
Managing stress, getting enough 7-to-9-hour sleep/night to stablise cortisol hormones and insulin.
Attending periodic endocrine follow-up when in high-risk group (family history, overweight, limited physical activities).
2. When the disease is already present
Personalised treatment objectives: HbA1c, blood pressure, lipid control according to age and underlying diseases.
Adhere to prescription and change lifestyle simultaneously
Smart blood glucose monitoring: utilizing Continuous Glucose Monitor (CGM) or regular monitoring
Multidisciplinary companion: endocrine – cardiovascular – kidneys – eyes – nutrition – psychology.
Personalised health education: patients comprehend the pathological mechanism, self-adjust diet-exercise-medication regimen daily.
Reference:
--------------------





























































Để lại bình luận