Thông báo
Vui lòng điền vào thông tin bên dưới
Khẩn cấp
72 GOLDEN HOURS IN THE MANAGEMENT OF SUDDEN SENSORINEURAL HEARING LOSS
Sudden Sensorineural Hearing Loss (SSNHL) is the rapid onset of sensorineural hearing loss, typically occurring within 72 hours (3 days) or less, with a loss of ≥ 30 dB at at least three contiguous audio frequencies on the audiogram.
Although many cases are idiopathic, SSNHL can lead to permanent hearing loss, affecting quality of life, communication, and balance (if accompanied by vestibular symptoms). It is considered an otologic emergency because delayed treatment can significantly reduce the chances of hearing recovery.
Classification
SSNHL is typically classified according to the following criteria:
1. By affected side
Unilateral: more common form
Bilateral: rare, often suggesting systemic causes or generalized disease
2. By degree of hearing loss / audiogram pattern
Mild, moderate, severe, profound loss (hearing level)
Audiogram pattern: typical (flat), high-frequency sloping, “U-shape”, etc.
Staging can be done according to HEAR criteria (H = hearing threshold, E = elapsed time from onset, A = audiogram shape, R = vestibular symptoms) — a staging method proposed in Johns Hopkins’s research to predict prognosis.
3. By etiology (if identifiable)
Idiopathic SSNHL accounts for the majority of cases.
Related to viruses, blood vessels, inner ear malformations, autoimmune conditions, inner ear trauma, or inner ear vasospastic disorders.
Due to systemic diseases (diabetes, lupus, anemia, atherosclerosis) if identified.
4. By timing of treatment initiation / expected response level
Early treatment (within 24–72 hours)
Delayed or late ( > 7 days)
Expected recovery: good / moderate / poor
Cause
While SSNHL has been extensively studied, it largely remains "idiopathic" (without a clear identifiable cause). However, commonly accepted hypotheses include:
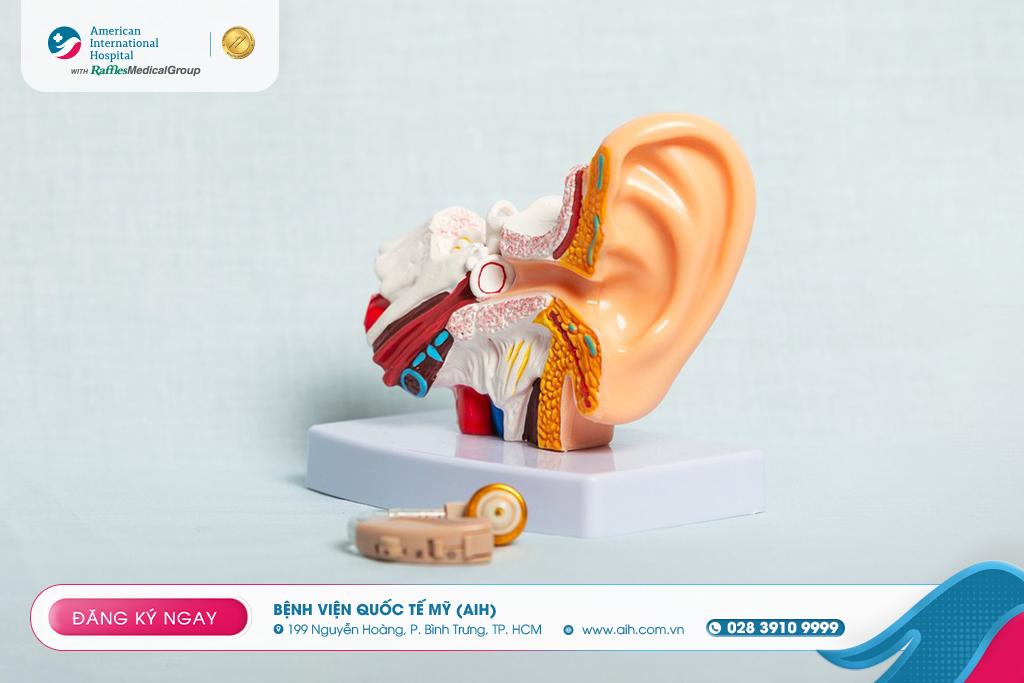
1. Vascular disorders / small vessel occlusion in the inner ear
Reduced microvascular perfusion or microvascular occlusion can cause ischemia to the hair cells in the cochlea. Some models suggest that vasoconstriction or small thrombi can affect inner ear circulation.
2. Viral impact / viral infections
Viral infections (e.g., influenza virus, herpes virus, other viruses) can cause inner ear inflammation or damage to hair cells. The inflammatory response can also lead to edema and diffuse lesion.
3. Membrane breaks / perilymphatic fistula
The hypothesis of perilymphatic fistula changes the pressure in the cochlea, causing damage to hair cells.
4. Autoimmune disorders / autoimmune inner ear inflammation
In some cases, an immune response may affect the inner ear tissue, leading to inflammation and damage to auditory nerve cells.
5. Other factors:
Vascular factors (atherosclerosis, hypertension)
Genetic factors / sensitive inner ear structure
Oxidative stress, free radicals
Certain ototoxic medications or systemic toxicity
Mechanical trauma or negative pressure
Symptoms
The typical clinical symptoms of SSNHL include:
Sudden hearing loss in one ear: the patient may wake up unable to hear in that ear or experience sudden hearing impairment within a few hours.
Tinnitus (ringing in the ear): often appears simultaneously or immediately after hearing loss.
May be accompanied by dizziness or loss of balance if the damage affects the vestibular system.
A feeling of pressure or fullness in the ear is sometimes described but is not typical.
No or little pain (unlike otitis media or ear infection): if there is pain, other causes should be considered.
Sometimes there are prodromal symptoms (e.g., a mild ringing sensation before complete hearing loss).
Some studies also show that when SSNHL is accompanied by vestibular symptoms or imbalance, the prognosis for recovery is often worse.
Diagnosis
Diagnosis of SSNHL includes the following steps:
1. History taking & clinical evaluation
Identify the onset of symptoms and their progression (sudden or over several hours/days).
Check for risk factors (diabetes, vascular disease, autoimmune disease, history of viral infection, trauma).
Examine the ear with an otoscope to rule out conductive causes (e.g., earwax impaction, abnormal eardrum).
Assess associated symptoms: tinnitus, dizziness, other neurological symptoms.
2. Audiometry
Perform pure-tone audiogram: measure hearing thresholds at multiple frequencies (air conduction and bone conduction) to determine the degree and type of hearing loss.
Commonly used criteria: loss of ≥ 30 dB at at least three consecutive frequencies within 3 days.
Compare bone conduction and air conduction to identify sensorineural damage if there is no conductive component.
3. Additional / exclusion tests
Tympanometry test to assess the middle ear if necessary.
If symptoms suggest a suspicious cause or severe/irreversible condition, an MRI of the ear / brain may be performed to rule out masses, acoustic neuroma (vestibulocochlear nerve tumor), and intracranial pathologies.
In cases of suspected inflammation or autoimmune conditions, hematological tests, inflammatory markers, antibodies, and vascular function tests may be performed.
Early intervention is crucial — late diagnosis (> 2 weeks) reduces treatment outcome.
4. Differentiate from other causes:
Conductive hearing loss (e.g., middle ear obstruction, fluid in the middle ear)
Mixed hearing loss
Chronic / progressive hearing loss
Central nervous system causes
Inner ear structural disorders (tumors, malformations)

Treatment
The treatment of SSNHL remains an area of significant debate, but the following principles are currently applied in practice:
1. General principles
Initiate treatment as early as possible (within 72 hours if feasible) to increase the likelihood of recovery.
Corticosteroids - either systemic or intratympanic injection - are the mainstay of primary treatment.
Monitor with periodic audiograms to assess improvement.
Provide symptomatic treatment (e.g., for vertigo, tinnitus).
In cases of non-response, consider adjunctive therapies.
2. Corticosteroid therapy
According to the Johns Hopkins "Quick Intervention Guide": use high-dose prednisone (e.g., 60 mg/day) for approximately 2 weeks, then taper the dose if there is a good response.
If systemic administration is not possible or if there is no improvement, intratympanic steroid injection (injecting steroids into the middle ear cavity, delivered through the eardrum) is considered an alternative or supplementary option.
3. Adjunctive / Other therapies
In studies / proposals: mild anticoagulants, vasodilators, and antioxidants (free radical scavengers) have been tested, but there is no strong evidence to recommend them generally.
In some cases with inflammation, antiviral treatment has been proposed, but its effectiveness has not been clearly demonstrated.
Supportive therapy: microcirculatory reperfusion, management of vascular factors (blood pressure control, diabetes mellitus).
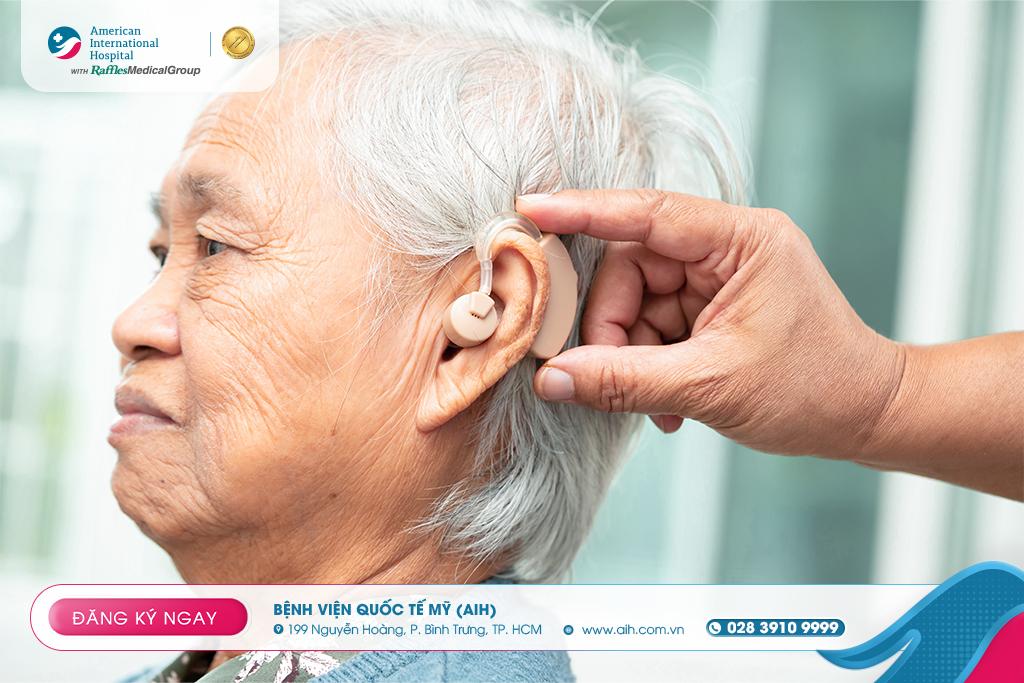
4. Monitoring & evaluating effectiveness
Perform repeat audiograms post-treatment to assess the degree of recovery.
If no improvement after the standard treatment period, consider further intervention (combination therapy, additional steroid injections, clinical trials)
Long-term management of residual symptoms (tinnitus, hearing support – using hearing aids if applicable), auditory rehabilitation.
Reference:
--------------------
Tìm kiếm
Tin tức
Bác sĩ





























































Để lại bình luận